The pain is generally a deep aching pain felt in the vicinity of the ball of the shoulder, but also commonly felt in the chest area and further down the arm to a point about midway between the shoulder and the elbow. The pain will often be present at rest and is generally more intense when one is using the arm and shoulder.
Stiffness will vary from very mild to extremely severe. An example would be stiffness so severe that one has difficulty reaching the middle belt loop on a pair of pants.
Sleep disturbance is a very common feature of idiopathic adhesive capsulitis. People find that they often awaken from sleep due to pain; they can generally return to sleep but are awakened again before their normal waking time. Sometimes changing position, using over-the-counter medication, or using ice will lessen the pain that is disturbing sleep.
Diagnosis
Diagnosing idiopathic adhesive capsulitis (frozen shoulder) requires a careful history. Certain features of the history as volunteered by the patient are very useful clues for the examiner. Does the shoulder hurt with sudden movements? Is the shoulder stiff? Have the symptoms been getting worse over the course of several weeks? These are all useful clues an examiner will seek.
Another important basic tool is a careful physical examination of both shoulders conducted by an experienced examiner. By combining the elements of a careful history, along with the findings of the physical exam, an examiner can narrow the possible causes of the patient’s shoulder pain and stiffness. It is often possible to reach a presumptive diagnosis of idiopathic adhesive capsulitis without sophisticated imaging studies.
Causes
The cause of adhesive capsulitis is unknown. There is a form of frozen shoulder that is associated with diabetes. If you are not a diabetic, please focus any research you may undertake on non-diabetic diagnosis of frozen shoulder.
It is common for patients to associate their early memories of shoulder pain with a specific task or event. This task may be an arm movement during a sporting event or a hard day of working in the yard. It is my belief that these memories are representative of symptoms present in a long evolution of frozen shoulder. The event remembered is probably not the actual cause of the frozen shoulder.
Treatment
Exercise is very effective at lessening the pain and stiffness of idiopathic adhesive capsulitis (frozen shoulder). It seems counterintuitive, but a lot of evidence shows that using a frozen shoulder helps it, and not using a frozen shoulder delays its recovery. Therefore, try to continue with your normal activities, like gardening or sports, as your tolerance allows. The intensity of your activity should be based on the level of pain you are able to tolerate.
Physical therapy is often employed in the treatment of idiopathic adhesive capsulitis. It may consist of a home exercise regimen and can also involve supervised physical therapy in combination with a home regimen.
A few patients will notice a decrease in stiffness and pain by treating frozen shoulder with cortisone injection; however, most patients do not notice substantial lasting relief. This is a treatment that I sometimes—but not generally—employ.
Over-the-counter pain medications designed to fight inflammation, such as Aleve or Advil, will sometimes lessen the pain and stiffness of frozen shoulder. I recommend that one try a seven to 10 day trial of over-the-counter anti-inflammatory medicines. If no relief is gained from this trial, I recommend that the patient stop using anti-inflammatory drugs for treatment of their frozen shoulder.
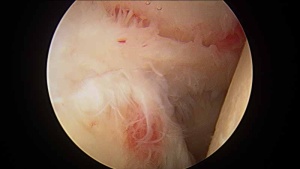
There is a role for surgery in patients with frozen shoulder who have failed to gain satisfactory relief of their pain or stiffness despite an adequate trial of nonoperative treatment. Surgery can include manipulation under anesthesia or arthroscopic frozen shoulder surgery. There are many important details to understand before making a decision about surgery for frozen shoulder.